This is the second installment in a series of articles exploring pertinent lab tests for people following low-carb diets, and how a slightly different perspective is needed when interpreting the results compared to results from people following high-carb diets.
In the previous post in this series, we looked at three measurements related to blood glucose: fasting glucose, hemoglobin A1c, and fructosamine. We left off saying that while these are important to monitor regularly, they offer a limited view of a much larger metabolic control system. Blood glucose, hemoglobin A1c (HbA1c), and fructosamine indicate only what’s happening with blood glucose. They reveal nothing about insulin, which we will explore in this post.
Knowing your numbers is an important step for anyone who wants to transform their health. Heads Up Health was designed to empower you to manage all of your health data, including your lab test results, in one secure location. You can learn more on our homepage or by clicking below to create your account and start building your own centralized health portfolio.
[maxbutton id=”4″]
The Fasting Insulin Test
We said it last time, and it’s worth repeating:
A fasting insulin test is the most important test your doctor probably isn’t ordering.
The reason it’s so important to track insulin is that in many cases, fasting glucose and A1c remain normal due to chronically elevated insulin—that is, sky-high insulin is keeping the glucose “in check.” Fasting glucose and HbA1c are often the last things to rise, and they become elevated only after one of two things has happened:
- The pancreas can no longer pump out the inordinate amounts of insulin required to keep blood glucose within a safe range (sometimes called “beta-cell burnout”). This is relatively rare, except in type-1 diabetes, which is an autoimmune condition and not driven by a poor diet.
- The pancreas still secretes large amounts of insulin but some of the body’s cells no longer respond to it properly, resulting in high blood glucose. (These cells become resistant to the presence of insulin.) This is far more common.
This explains why many people are surprised by a diagnosis of type 2 diabetes or pre-diabetes. They—and their doctors—had been lulled into a false sense of security by glucose measurements that fell within normal ranges for years, because no one was measuring insulin.
Medical professionals who are aware of the wide-ranging effects of chronically elevated insulin would agree that a fasting insulin test should be included as a standard part of routine bloodwork. But until that happens, if you’re concerned with getting and remaining metabolically healthy, you will need to specifically request it from your doctor or order it on your own from a direct-to-consumer lab testing service.

Insulin helps control blood glucose.
Here’s how to use a fasting insulin test as a gauge for metabolic health:
- Optimal range: 1- 9 μU/mL
- Intermediate risk range: 10 -11 μU/mL
- High risk range: ≥ 12 μU/mL
If your fasting insulin is in the double digits, it’s a sure sign something is awry. However, just as we explained regarding fasting glucose, if your fasting insulin falls within the optimal range, it doesn’t automatically mean everything’s fine. In some people, the fasting level is normal, but the level after meals rises very high and takes an extended length of time to come back to baseline—if it even does come down fully before the next meal. So it’s possible to have a fasting insulin level in the optimal range but have high insulin throughout most of the rest of the day.
Chronically elevated insulin ( called “hyperinsulinemia”) should be suspected when fasting glucose, HbA1c, and possibly fasting insulin are normal, but you experience unexplained or “idiopathic” health issues, such as:
- Stubborn fat loss
- Hypertension (high blood pressure)
- Headaches; migraines
- Gout
- Skin tags
- Vertigo
- Tinnitus
- Infertility (in women and men)
- Erectile dysfunction
- Benign prostatic hyperplasia
- Polycystic ovarian syndrome (PCOS)
- Gynecomastia (enlargement of breast tissue in males)
Unfortunately, owing to the complexity of the chemical assay used to measure insulin, there’s currently no way to measure insulin at home, the way you can do with glucose and HbA1c.
Why Track Insulin?
Medical professionals—particularly physicians, nutritionists, and researchers who work with individuals with obesity, type-2 diabetes, and metabolic syndrome—increasingly recognize that it is elevated insulin, rather than blood glucose, that’s responsible for many of the chronic illnesses that plague millions of people, robbing them of quality and quantity of life. Chronically elevated blood glucose (“hyperglycemia”) is dangerous and, over time, results in damage to the eyes, kidneys, liver, blood vessels, and extremities. Much of the organ and tissue damage that occurs in type-2 diabetics with poor blood sugar control results from chronic hyperglycemia.
But, many non-diabetics will experience physical deterioration in the absence of high blood glucose. In these individuals, it’s the insulin that’s the problem. These folks are essentially diabetic, but because their blood glucose is normal, they won’t be officially diagnosed. This is what Dr. Joseph Kraft called “diabetes in-situ,” or “occult diabetes”—occult, meaning hidden. The high blood sugar is hidden or masked by the pathologically high insulin.
A large and still growing body of scientific research indicates that chronic hyperinsulinemia is the unifying factor behind some of the most common chronic illnesses of our time. Michael Eades, MD, Mary Dan Eades, MD, and Loren Cordain, PhD, some of the earliest proponents of low-carb and Paleo diets, explained over a decade ago that hyperinsulinemia may be the driving force behind acne, skin tags, PCOS, myopia, and male pattern baldness (it’s not all genetic!). Chronically elevated insulin is also a risk factor for Alzheimer’s disease, infertility, and sexual dysfunction, inner-ear and balance disorders (e.g., vertigo, tinnitus, Ménière’s disease), some forms of cancer (coupled with worse prognosis in those undergoing treatment), and cardiovascular disease. In fact, Dr. Kraft wrote, “Those with cardiovascular disease not identified with diabetes are simply undiagnosed.”

Want to stay healthy? Measure insulin!
Something to keep in mind is that hyperinsulinemia occurs in people of all shapes and sizes. Obesity is more often an effect, rather than a cause, of disturbed insulin and glucose signaling in the body. So individuals who are lean and appear healthy on the outside are not immune to the adverse effects of high insulin. These individuals have personal body fat set points that prevent them from becoming overweight or obese, but they’re not spared the other undesirable outcomes from derailed metabolism. (Researchers call this “normal weight obesity,” but more casually it’s referred to as TOFI – thin outside, fat inside. Even though these folks remain at a “normal” weight, their biomarkers indicate metabolic syndrome or insulin resistance.)
Tracking insulin is the canary in the coal mine – the “check engine light.” It’s an early warning sign that your diet and lifestyle need adjustments. You don’t have to wait until your blood glucose is high enough to prompt a type-2 or pre-diabetes diagnosis. Elevated fasting insulin might be one of the first indicators that something’s amiss, and you can take action to correct it.
Track your progress
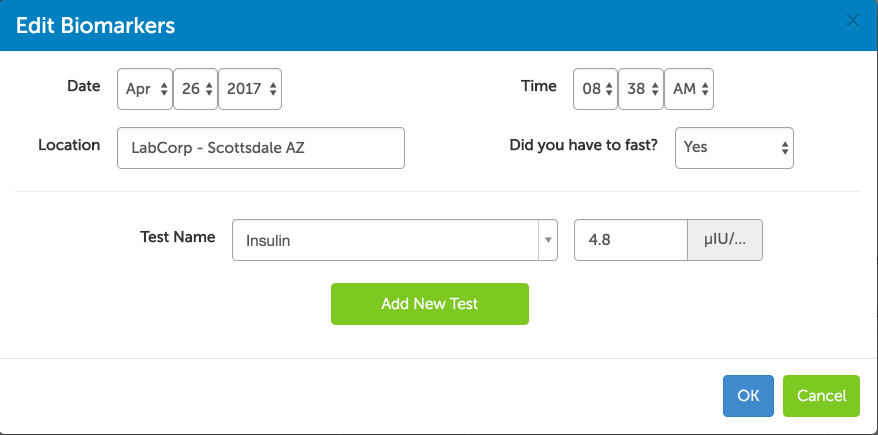
The Heads Up Health app was designed specifically for individuals to take control of their health data so it can be used for better decision-making. For our users within the United States, you can electronically link your medical facility to your Heads Up account and instantly import your lab test results. If we can’t connect to your medical facility or you live outside the US, you can easily enter your results manually:
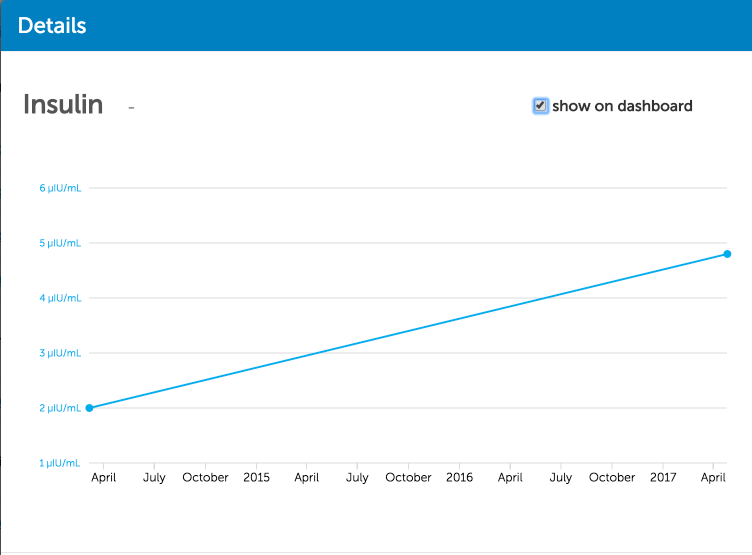
With subsequent tests, you can also trend your results over time to see how your low-carb lifestyle is impacting important markers like fasting insulin:
Heads Up can also integrate the data you are collecting at home – everything from weight to blood sugar and steps per day – so you can compare how your healthy lifestyle choices are impacting your lab test results.
[maxbutton id=”4″]
Coming up next…
In the next post, we’ll introduce you to the HOMA-IR test that will help you connect your fasting insulin and glucose levels for a deeper analysis of your level of metabolic health.










How to control my glicemic index in the morning?
It’s low all day and high in the am.
I have been on low carb diet for two years. Fasting insulin ranged from 4 to 8 in tests six months and earlier. However, it was 0.8 in the most recent test. Should I be concerned that it gets this low? Thank you!