by Heads Up Health | May 18, 2017 | Self Tracking
Let’s face it: if you’re concerned about your health, you’ve got to take matters into your own hands. Between battling your insurance company, working with an uncooperative doctor, and going up against outdated dietary advice that’s dying far too slow a death, if you want to attain and maintain optimal metabolic health, sometimes you have to get in the driver’s seat and order your own lab tests.
Doctors are intelligent, hardworking, and dedicated people, but they’re not infallible. Between seeing patients, dealing with burdensome paperwork, and overseeing the day-to-day operation of their offices, many of them have precious little time left for staying up-to-date on the latest research in their fields. And even if they’re keeping current with developments in their particular specialty, they might remain unaware of breakthroughs in other disciplines that could have important implications for their own—and for your health.
What this means is, if you’d like to run your labs more frequently than your doc is inclined to order them for you, or you want to get some lab tests your doctor isn’t familiar with, you have to go a different route.
In this post, we’ll show you how to run your own labs so you can obtain the information you need to feel in control of your health. We will also show you how Heads Up Health can help you manage all of your health data, including lab test results, in one single and secure location. You can learn more about the Heads Up Health service by clicking on the button below. Or, read on for more information on how you can take control of your health by running your own lab tests.
[maxbutton id=”6″]
Reasons to Order Your Own Lab Tests
- Uncooperative doctors: If you request certain tests from your doctor because your own research has led you to believe they’d give you valuable information, don’t be surprised if the doc doesn’t share your enthusiasm. Even if you present them with an armload of studies from reputable scientific journals to support your case, your doctor still might not be keen on ordering anything and everything you request. For better or worse, lots of folks consult “Dr. Google” these days, and while there’s a world of helpful information regarding health and wellness to be found online, there’s also a lot that’s misleading, confusing, and just plain wrong. So you can’t blame your doctor for hesitating. While you’re the expert on your own body, he or she is the expert when it comes to medicine. So if your doctor is uncooperative, it’s not because they’re stubborn and enjoy giving you a hard time. More likely it’s that they’re simply not aware of the importance of some of the tests you might ask for. (Case in point: fasting insulin—the most important test doctors aren’t ordering.)
- You want to test more frequently than your insurance covers: When you make changes to your diet and lifestyle, good things start happening fast. For example, blood glucose, insulin, and blood pressure can decrease dramatically within just a few days of starting a low-carb diet. Other favorable changes take only a few weeks. But maybe your insurance covers a checkup and routine bloodwork only every six months, or once a year. You don’t want to wait that long. Seeing for sure that your triglycerides have come down or you’ve got much less inflammation could encourage you to stick with whatever plan you’re following. Nothing motivates more than results.
- Insurance doesn’t cover the tests you want: Insurance companies aren’t in the habit of paying for anything they don’t deem absolutely necessary. So if you’re looking for tests outside the mainstream—an advanced cholesterol panel, for example—you’re often on your own.
- You want a test that falls outside the conventional offerings: Food sensitivity tests, organic acid profiles, stool testing, and other tests that are well-known within the low-carb, ketogenic, and Paleo/ancestral health communities aren’t exactly household words. Many doctors wouldn’t even know how to order these for you. If you want this kind of cutting-edge testing—perhaps to get answers to longstanding health concerns that have not resolved after exhausting other options—you’ll need to find a private company that offers them.
So what’s a concerned patient to do?

Be proactive — get lab tests done on your own!
Good news! There are now several options available for you to order your own lab tests—no referral required! You can order the tests you’d like, print out the requisition, and visit a lab to have your blood or urine sample collected. The results are sent directly to you (usually electronically, through an account you create with the testing company).
The companies that provide these services typically don’t accept payment by insurance, but they can provide you with a detailed receipt or medical CPT codes so you can file for reimbursement from your insurance company. (Be sure to check with your provider; not all insurance companies will reimburse for this.)
Don’t let an uncooperative doctor or a stingy insurance company be a roadblock to gathering data you feel is important for your health. Remember: Nobody cares about your health more than you do. But you can’t track things if you don’t have the data, and you won’t have the data without running lab tests.
Here are five companies providing direct-to-consumer lab tests:
Note: When you purchase lab tests from Request-a-Test, DirectLabs, InsideTracker, or MyMedLab, they will direct you to Quest Diagnostics to have the blood drawn and analyzed. The good news is Quest Diagnostics is already integrated with Heads Up Health. This means you can connect Quest Diagnostics to your Heads Up profile and your lab test results will instantly synchronize. See this video for more information on connecting Quest Diagnostics to your Heads Up account or contact us if you need assistance.
Tracking your results
Heads Up Health was designed to help you track all of your vital health data in one place, including your lab test results, so you can have a complete picture of your health available at all times. With connections to over 20,000 health systems across the US, you can easily integrate your lab test results into your Heads Up profile and track your results over time. You can also track your blood sugar, ketones, body composition, and other important health metrics so you can better understand how your lifestyle changes are affecting your overall health.

Track your blood sugar test results with Heads Up Health
If you are ready to start taking control of your health data, create an account using the button below. You can also contact us any time with any questions or find us on Facebook, Twitter, and YouTube for our latest updates.
[maxbutton id=”4″]

by Heads Up Health | May 14, 2017 | Self Tracking
This is the third installment in a series of articles exploring lab tests for people following low-carb diets, and how this way of eating requires a slightly different perspective for interpreting the results compared to results from people eating more carbohydrates.
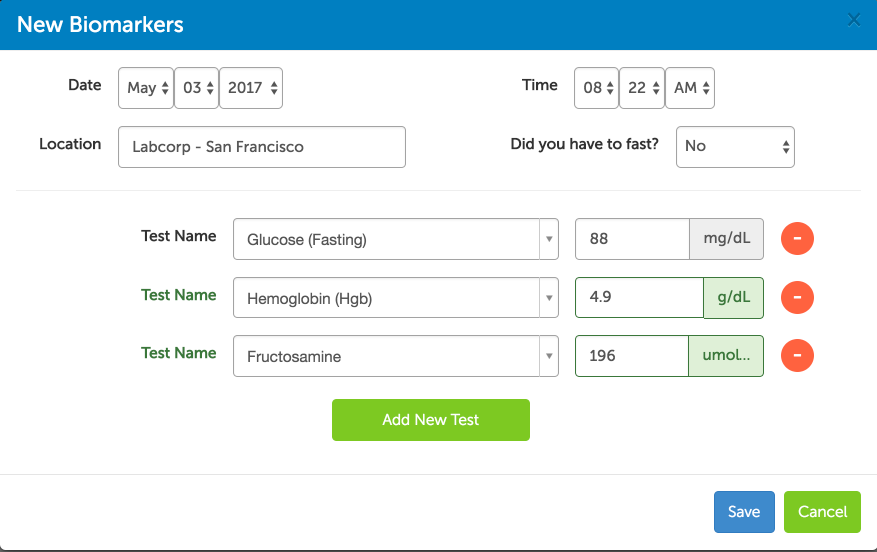
In part 1, we covered tests for blood sugar (fasting glucose, hemoglobin A1c, and fructosamine). In part 2, we explored fasting insulin, the most important test most doctors aren’t ordering. Taken together, these explain why fasting glucose and hemoglobin A1c in the “normal” ranges don’t always mean someone’s in the clear with regard to insulin sensitivity and healthy glucoregulation. (Crash course: for many people, dangerously high insulin is the only thing keeping glucose levels in a healthy range.)
Throughout this series, we’re emphasizing that health cannot be determined by any single measurement in isolation. It’s a mosaic, made up of many individual parts that are best assessed as a whole. With this in mind, let’s dig a little deeper into the relationship between glucose and insulin. (more…)

by Heads Up Health | Mar 29, 2017 | Self Tracking
This is the second installment in a series of articles exploring pertinent lab tests for people following low-carb diets, and how a slightly different perspective is needed when interpreting the results compared to results from people following high-carb diets.
In the previous post in this series, we looked at three measurements related to blood glucose: fasting glucose, hemoglobin A1c, and fructosamine. We left off saying that while these are important to monitor regularly, they offer a limited view of a much larger metabolic control system. Blood glucose, hemoglobin A1c (HbA1c), and fructosamine indicate only what’s happening with blood glucose. They reveal nothing about insulin, which we will explore in this post.
Knowing your numbers is an important step for anyone who wants to transform their health. Heads Up Health was designed to empower you to manage all of your health data, including your lab test results, in one secure location. You can learn more on our homepage or by clicking below to create your account and start building your own centralized health portfolio.
[maxbutton id=”4″]
The Fasting Insulin Test
We said it last time, and it’s worth repeating:
A fasting insulin test is the most important test your doctor probably isn’t ordering.
The reason it’s so important to track insulin is that in many cases, fasting glucose and A1c remain normal due to chronically elevated insulin—that is, sky-high insulin is keeping the glucose “in check.” Fasting glucose and HbA1c are often the last things to rise, and they become elevated only after one of two things has happened:
- The pancreas can no longer pump out the inordinate amounts of insulin required to keep blood glucose within a safe range (sometimes called “beta-cell burnout”). This is relatively rare, except in type-1 diabetes, which is an autoimmune condition and not driven by a poor diet.
- The pancreas still secretes large amounts of insulin but some of the body’s cells no longer respond to it properly, resulting in high blood glucose. (These cells become resistant to the presence of insulin.) This is far more common.
This explains why many people are surprised by a diagnosis of type 2 diabetes or pre-diabetes. They—and their doctors—had been lulled into a false sense of security by glucose measurements that fell within normal ranges for years, because no one was measuring insulin.
Medical professionals who are aware of the wide-ranging effects of chronically elevated insulin would agree that a fasting insulin test should be included as a standard part of routine bloodwork. But until that happens, if you’re concerned with getting and remaining metabolically healthy, you will need to specifically request it from your doctor or order it on your own from a direct-to-consumer lab testing service.

Insulin helps control blood glucose.
Here’s how to use a fasting insulin test as a gauge for metabolic health:
- Optimal range: 1- 9 μU/mL
- Intermediate risk range: 10 -11 μU/mL
- High risk range: ≥ 12 μU/mL
If your fasting insulin is in the double digits, it’s a sure sign something is awry. However, just as we explained regarding fasting glucose, if your fasting insulin falls within the optimal range, it doesn’t automatically mean everything’s fine. In some people, the fasting level is normal, but the level after meals rises very high and takes an extended length of time to come back to baseline—if it even does come down fully before the next meal. So it’s possible to have a fasting insulin level in the optimal range but have high insulin throughout most of the rest of the day.
Chronically elevated insulin ( called “hyperinsulinemia”) should be suspected when fasting glucose, HbA1c, and possibly fasting insulin are normal, but you experience unexplained or “idiopathic” health issues, such as:
- Stubborn fat loss
- Hypertension (high blood pressure)
- Headaches; migraines
- Gout
- Skin tags
- Vertigo
- Tinnitus
- Infertility (in women and men)
- Erectile dysfunction
- Benign prostatic hyperplasia
- Polycystic ovarian syndrome (PCOS)
- Gynecomastia (enlargement of breast tissue in males)
Unfortunately, owing to the complexity of the chemical assay used to measure insulin, there’s currently no way to measure insulin at home, the way you can do with glucose and HbA1c.
Why Track Insulin?
Medical professionals—particularly physicians, nutritionists, and researchers who work with individuals with obesity, type-2 diabetes, and metabolic syndrome—increasingly recognize that it is elevated insulin, rather than blood glucose, that’s responsible for many of the chronic illnesses that plague millions of people, robbing them of quality and quantity of life. Chronically elevated blood glucose (“hyperglycemia”) is dangerous and, over time, results in damage to the eyes, kidneys, liver, blood vessels, and extremities. Much of the organ and tissue damage that occurs in type-2 diabetics with poor blood sugar control results from chronic hyperglycemia.
But, many non-diabetics will experience physical deterioration in the absence of high blood glucose. In these individuals, it’s the insulin that’s the problem. These folks are essentially diabetic, but because their blood glucose is normal, they won’t be officially diagnosed. This is what Dr. Joseph Kraft called “diabetes in-situ,” or “occult diabetes”—occult, meaning hidden. The high blood sugar is hidden or masked by the pathologically high insulin.
A large and still growing body of scientific research indicates that chronic hyperinsulinemia is the unifying factor behind some of the most common chronic illnesses of our time. Michael Eades, MD, Mary Dan Eades, MD, and Loren Cordain, PhD, some of the earliest proponents of low-carb and Paleo diets, explained over a decade ago that hyperinsulinemia may be the driving force behind acne, skin tags, PCOS, myopia, and male pattern baldness (it’s not all genetic!). Chronically elevated insulin is also a risk factor for Alzheimer’s disease, infertility, and sexual dysfunction, inner-ear and balance disorders (e.g., vertigo, tinnitus, Ménière’s disease), some forms of cancer (coupled with worse prognosis in those undergoing treatment), and cardiovascular disease. In fact, Dr. Kraft wrote, “Those with cardiovascular disease not identified with diabetes are simply undiagnosed.”

Want to stay healthy? Measure insulin!
Something to keep in mind is that hyperinsulinemia occurs in people of all shapes and sizes. Obesity is more often an effect, rather than a cause, of disturbed insulin and glucose signaling in the body. So individuals who are lean and appear healthy on the outside are not immune to the adverse effects of high insulin. These individuals have personal body fat set points that prevent them from becoming overweight or obese, but they’re not spared the other undesirable outcomes from derailed metabolism. (Researchers call this “normal weight obesity,” but more casually it’s referred to as TOFI – thin outside, fat inside. Even though these folks remain at a “normal” weight, their biomarkers indicate metabolic syndrome or insulin resistance.)
Tracking insulin is the canary in the coal mine – the “check engine light.” It’s an early warning sign that your diet and lifestyle need adjustments. You don’t have to wait until your blood glucose is high enough to prompt a type-2 or pre-diabetes diagnosis. Elevated fasting insulin might be one of the first indicators that something’s amiss, and you can take action to correct it.
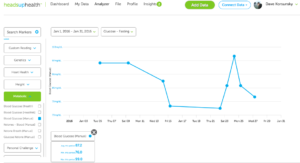
Track your progress
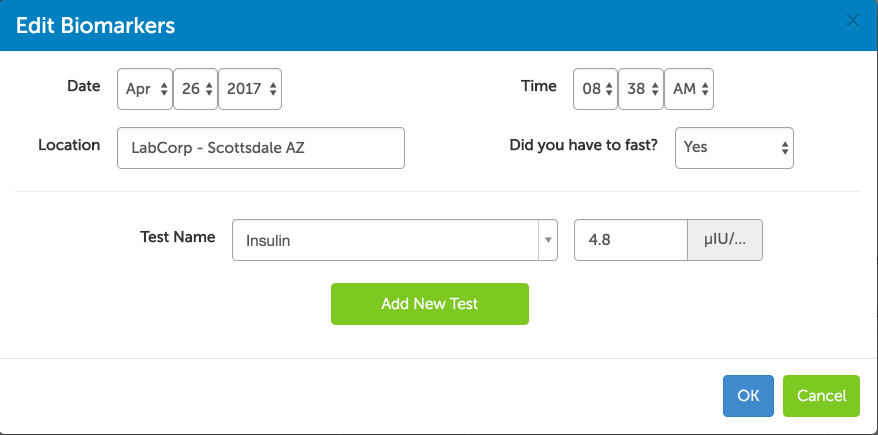
The Heads Up Health app was designed specifically for individuals to take control of their health data so it can be used for better decision-making. For our users within the United States, you can electronically link your medical facility to your Heads Up account and instantly import your lab test results. If we can’t connect to your medical facility or you live outside the US, you can easily enter your results manually:
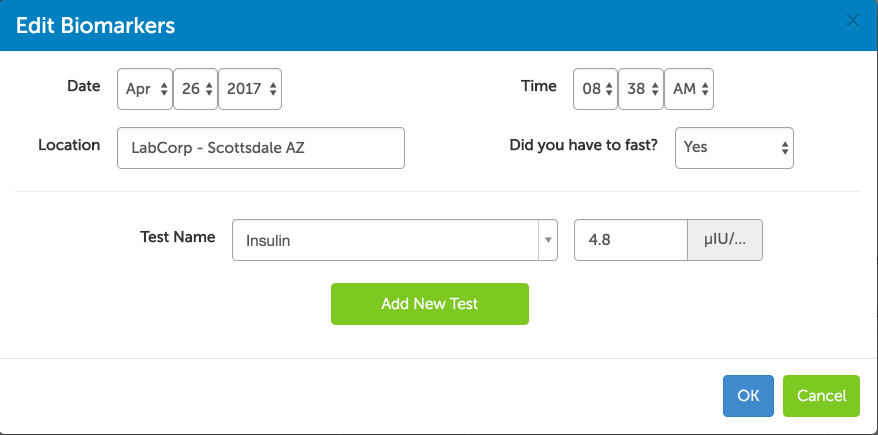
Track your fasting insulin results with Heads Up Health
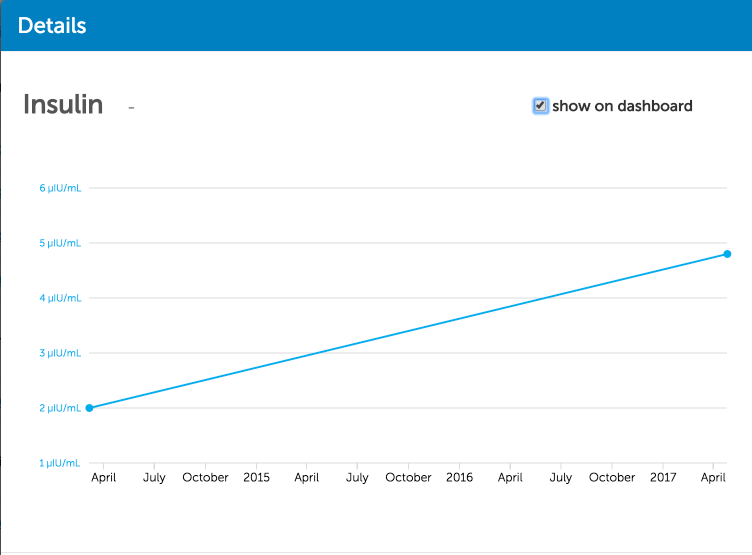
With subsequent tests, you can also trend your results over time to see how your low-carb lifestyle is impacting important markers like fasting insulin:
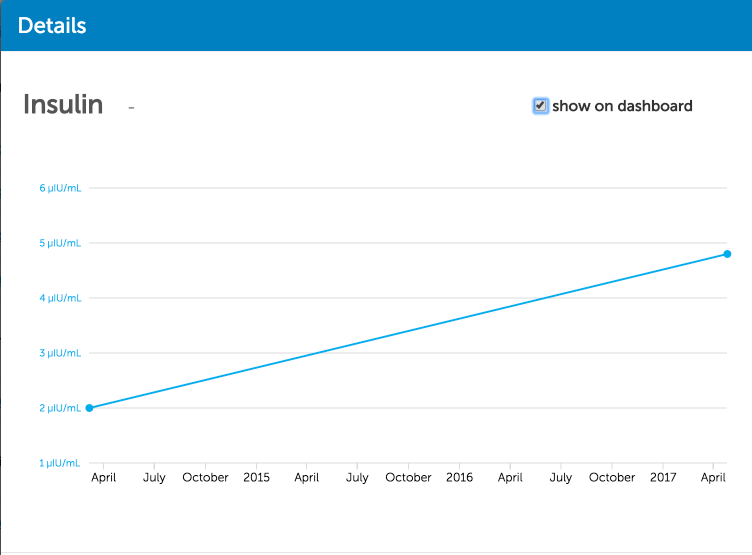
Trending your fasting insulin results over time
Heads Up can also integrate the data you are collecting at home – everything from weight to blood sugar and steps per day – so you can compare how your healthy lifestyle choices are impacting your lab test results.
[maxbutton id=”4″]
Coming up next…
In the next post, we’ll introduce you to the HOMA-IR test that will help you connect your fasting insulin and glucose levels for a deeper analysis of your level of metabolic health.

by Heads Up Health | Mar 2, 2017 | Self Tracking
Welcome to part 1 of our series on low-carb lab testing. In this first post, we look at three tests that can be used to monitor your blood glucose levels. In subsequent posts, we’ll shift focus to insulin, lipids, thyroid and other markers that are important for patients to understand. We’ll help you understand what these tests mean and how to track your results so you are in the driver’s seat when it comes to you health!
Heads Up Health is a web app designed to help you centrally track all of your vital health data – including your blood test results. Instantly synchronize your medical records, connect your favorite health devices and apps and use your data to optimize your health! Click on the button below to create your account. Or, read on for more information about common tests to help you monitor your blood sugar levels.
[maxbutton id=”5″]
Blood sugar, insulin and health
Chronic, long term pathological elevations in blood glucose or insulin have been linked to type 2 diabetes, obesity, Alzheimer’s disease, kidney problems, deterioration of eyesight, neuropathy, poor prognosis in cancer, connective tissue irregularities, orthopedic injuries and more. Links and associations are not necessarily causal relationships, but the medical literature is robust with research detailing potential mechanisms by which chronically high blood glucose or insulin might be either directly causing or at the very least exacerbating these outcomes. With this in mind, if you’re concerned about your long term health and quality of life, keeping blood glucose and insulin within healthy ranges is one of the most important and effective things you can do.
There are a number of blood tests that can help you keep track of your glycemic control. Results within the healthy ranges can keep you on the straight and narrow, while results that fall outside the optimal range can serve as a wakeup call if you need to be nudged back onto the path. Here we’ll look at few of the relevant tests and determine their proper place in helping you ensure optimal health and graceful aging.
Before we get into things, though, keep this in mind: your health is a mosaic, not a snapshot. It’s a whole picture, made up of many interrelated and interdependent factors. You should neither become alarmed nor rest assured based on any one measurement in isolation. Rather, you and your healthcare team should consider the sum total of the interactions that contribute to your overall health status. It’s easy to get a false sense of security—or become unnecessarily worried—based on one single measurement of any of the parameters below. So, for each one, we’ll tackle what it is, what it means, and why a high or low reading might be misleading.
Fasting blood glucose

Blood sugar test – fasting glucose
This is exactly what it sounds like—a measurement of your blood glucose level after it’s been about 8-12 hours since you’ve last eaten. (It’s typically performed in the morning, after an overnight fast.)
According to criteria from the American Diabetes Association (ADA), the following fasting blood glucose levels indicate pre-diabetes or diabetes:
- Pre-diabetes: ≥ 100-125 mg/dL (5.6 – 6.9 mmol/L)
- Type 2 diabetes: > 126 mg/dL (7.0 mmol/L)
However: a fasting level of less than 100 mg/dL (5.5 mmol/L) doesn’t automatically mean you’re in the clear, good to go, and all that jazz. A fasting glucose measurement is just a snapshot in time—one measurement at one moment. Unless it’s very high, it’s hard to take away any definitive information from this. Fasting blood glucose can be elevated for a couple of reasons that are not indicators of diabetes:
- Stress: Don’t underestimate the impact of stress on blood sugar. If you were stuck in a traffic jam or had a hectic morning before arriving at the lab, your blood sugar might be higher than it otherwise would have been, and it’s because of the aggravation, not because you’re careening toward a type 2 diabetes diagnosis. Feeling especially nervous around doctors or phlebotomists (“white coat syndrome”) may also play a role.
- Low carb diets: Fasting blood glucose might be slightly higher than expected in people who’ve been following a low carbohydrate or ketogenic diet for a significant amount of time. This is sometimes referred to as “physiological insulin resistance,” but a more descriptive phrase is “adaptive glucose sparing.” What it means is that in people whose metabolisms are primarily powered by fat, rather than glucose (they are “fat adapted”), the muscles and many of the body’s other tissues preferentially run on fat and ketones, thus “sparing” glucose for the tissues with an absolute requirement for it, such as the brain, red blood cells, and select other cells. In this case, the slight elevation in fasting glucose is to be expected and is not considered pathological.
So how do you know whether a slightly elevated fasting glucose is problematic? This brings us to our next test.
[maxbutton id=”5″ url=”https://headsuphealth.com” text=”Track Your Lab Tests!” ]
Hemoglobin A1C
This is a measurement of the average blood glucose over approximately the previous two to three months. (Hemoglobin is a protein in red blood cells that contains iron and transports oxygen. This test measures glycated hemoglobin – hemoglobin that has become “sticky” with glucose.) This is a more reliable test than fasting glucose for indicating abnormalities in glycemic control. If your fasting glucose is slightly high but your A1c is optimal, then one of the above non-pathological reasons might explain your higher fasting reading.
Blood sugar test – Hemoglobin A1c
Here’s how the ADA classifies hemoglobin A1c with regard to indicating diabetes:
- Pre-diabetes: 5.7-6.4%
- Type 2 diabetes: ≥ 6.5%
Most low-carb savvy doctors would prefer to see A1c below 5.5%. However, just like with the fasting reading, there are reasons why A1c isn’t always a reliable marker:
- Low carb diets: Good health strikes again! The reason A1c is considered to measure a two to three (or four) month average blood glucose is because the lifespan of red blood cells is typically 100-120 days. But red blood cells (RBCs) that are especially healthy and hardy might stick around a bit longer, which gives them more time to become glycated. So with a slightly elevated A1c, we have yet another measurement that could be alarming if taken out of its proper context. Individuals following low carb or ketogenic diets for a while might have long-lived RBCs, and thus a higher A1c than they would expect based on their diet and lifestyle. If you check your blood glucose regularly and rarely or never see it elevated into hyperglycemic territory but have a higher A1c than you would expect, this is likely the reason.
- Anemia: Individuals with anemia (including sickle cell anemia) have red blood cells with shorter lifespans and thus might have an artificially low A1c reading. (Any other condition that shortens RBC survival time or increases RBC turnover can also result in a falsely low A1c.)
Great. So neither fasting glucose nor A1c can always be relied upon? What now?
Well, if your fasting glucose or A1c reading surprises you and you’d like some reassurance that you’re not headed into choppy seas, there’s another test that can put your mind at ease:
Fructosamine
This is a helpful test to include if your A1c is known or suspected to be unreliable. This test is similar to the A1c, but rather than an average blood glucose over the previous few months, fructosamine indicates glycemic control during the previous 2-3 weeks. Fructosamine is a compound formed when glucose combines with certain proteins, such as albumin, which is the most abundant protein in blood. Proteins exist in the blood for less time than the lifespan of a red blood cell. They’re around for about 14 to 21 days, so the glycated proteins the fructosamine test measures reflect average glucose levels during this timeframe. Some tests assess the glycation of total serum proteins, while others assess the glycation of albumin, specifically. (Some labs use the name Glycated Serum Protein [GSP] rather than fructosamine.)
There are currently no widely accepted standard reference ranges for fructosamine. The reference values depend on a person’s age, gender, and the testing method employed.
That being said, Johns Hopkins Medical Center offers the following ranges for fructosamine:
- Non-diabetic: 175-280 mmol/L
- Controlled diabetes: 210-421 mmol/L
- Uncontrolled diabetes: 268-870 mmol/L
In addition to giving a good picture of glycemic control when fasting glucose or A1c is unreliable, fructosamine is also helpful for guiding changes in diabetes treatment. Because it reflects changes that occur within weeks, rather than months, it’s useful for gauging the efficacy of changes in diet, medication, and lifestyle.
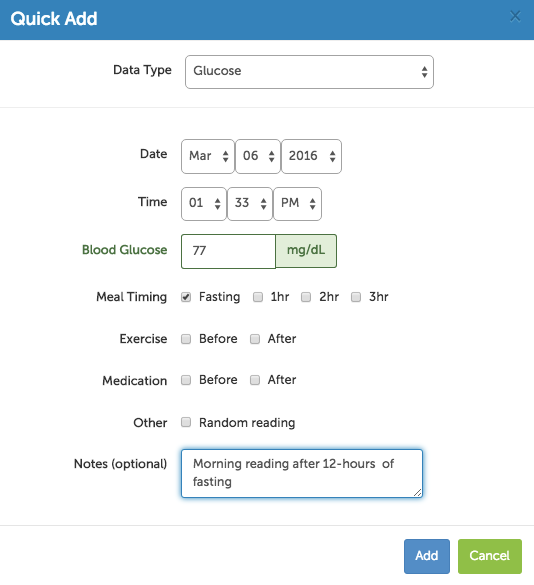
Tracking your progress
Heads Up Health was designed to help you manage all of your health data in one place so you can see the big picture when it comes to your low-carb lifestyle. If you are testing your blood sugar at home with a glucometer, you can easily track this data within your Heads Up Health profile:
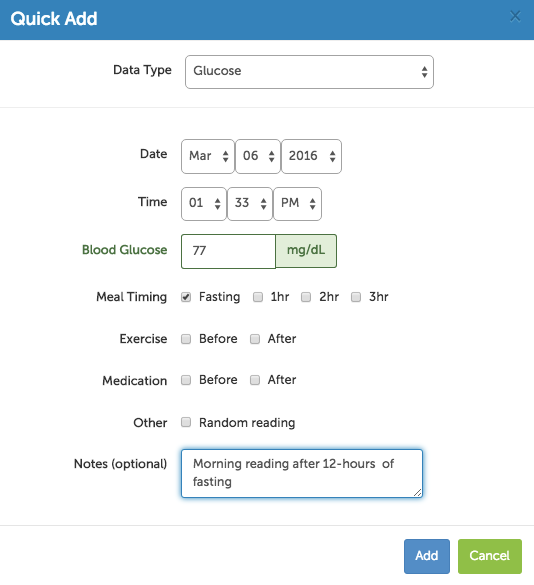
Blood sugar testing – track your progress with Heads Up Health
Heads Up can also integrate your lab test results so you can see how your low-carb lifestyle is affecting metrics like hemoglobin A1c and fructosamine:
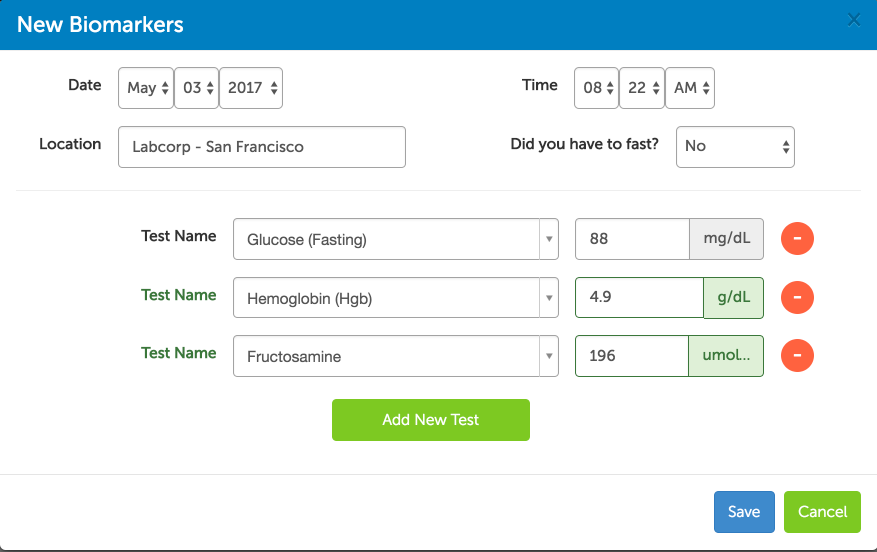
Track your lab test results
You can also track your blood sugar, ketones, body composition and any other health metrics that are important to you. Click the button below to create your account and start tracking your results!
[maxbutton id=”5″ ]
What to Do About All This
We’ve taken a look at some of the most common tests that can be used to monitor your blood glucose. We’ve also covered some reasons why these markers of blood glucose control might be a bit higher or lower than you’d expect. But what about when they’re normal? If your fasting glucose, A1c, and fructosamine are all normal, can you sit back, relax, and keep on keepin’ on’?
The obvious—and easy—answer to this is yes. But like so much in medicine and science, the obvious and easy answer isn’t always the right answer. The truth is, even if all those measurements look good, something else could throw your health for a loop. Because there’s one thing—a very big thing—that none of those tests measure. Fasting glucose, A1c, and fructosamine are all measures of what’s happening with glucose. They tell you nothing about insulin. Fasting insulin is the most important test your doctor probably isn’t ordering.
And if you are ready to start tracking your own lab test results, click the button below to start your free trial for Heads Up Health. We’ll empower you with the data you need to master your health!
[maxbutton id=”4″]
Stay tuned. We’ll look at measuring insulin—and why it’s so important—in our next post in this series.

by Dave Korsunsky | Sep 4, 2016 | Self Tracking
Blood sugar testing is a relatively simple process that can reveal a wealth of valuable information about your health. From early detection of diabetes (and pre-diabetes) to healthy weight loss and stable energy levels, we recommend that all Heads Up Health users complete some basic testing to understand their blood sugar. (more…)

by Dave Korsunsky | Feb 7, 2016 | Self Tracking
At the start of 2016, I decided to resume my own n=1 experiment on the ketogenic diet. I’d tested this diet briefly back in October 2015 and had some encouraging results. Most notably, I lost weight, my fasting blood sugar came down, I had incredible amounts of energy and my mental acuity and performance felt better than ever. Simply put, my first experience with ketosis was the best I’ve felt in years. I wanted more!
Therefore, as of the beginning of this year, I’ve been focused on getting back into a state of nutritional ketosis. I’ll be sharing my results over the course of the experiment here on the blog. All my data – from blood sugar levels to lab test results – is tracked in the Heads Up Health app. If you’d like to get started doing the same, click the link below.
[maxbutton id=”4″]
Blood Sugar
The first interesting observation is the change in my fasting blood sugar(i). To induce a state of nutritional ketosis I had been limiting my carbohydrate intake to 5% of my total calories per day (about 20 grams of total carbs daily). Not surprisingly, my fasting blood sugar plummeted (click to enlarge image):
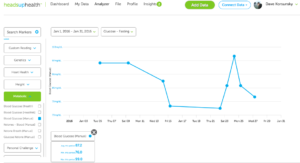
Fasting Blood Sugar on Ketogenic Diet
Observations from this graph:
- My fasting sugar dropped from 96 mg/dL down to 81 mg/dL by the end of the month. At one point it even dipped down into the high 70’s. For those looking to control blood sugar, the ketogenic diet is certainly highly effective here.
- There was one spike at 99 mg/dL on Jan 24th. I checked my nutrition logs and sure enough I had consumed a good handful of refined carbs the night before when I was out for dinner with friends.
- Fasting sugar came back down for the remainder of the month as I got back onto a disciplined ketogenic diet
Weight
I’ve been tracking weight(ii) regularly and have been looking forward to dropping some unwanted body fat over the course of the experiment. One of the benefits of nutritional ketosis is the weight loss that comes with it as your body begins to burn fat for fuel. Taking a look at my weight readings, I was pleased with the results (click the graph to enlarge):

Tracking weight and fasting blood sugar on ketogenic diet
Observations from this graph:
- My weight dropped from 197.2 pounds to 192.6 pounds which is a respectable 4.6 pounds lost in the month.
- This just over one pound lost per week, which is about right for ketosis based on my early understanding of the diet.
- Fluid loss can account for about 5-10% of the initial weight loss on keto. Therefore, it will be important to keep an eye on the scale over time as my body’s fluid levels normalize.
- I’ve also graphed fasting blood sugar on the graph along with weight. The two appear to be correlated based on these early measurements.
Body fat percentage
Equally, if not more important than weight is body fat percentage(iii). Even if my weight is increasing, as long as body fat percentage is going down, I know that I am losing fat and my overall body composition is improving:

Tracking weight and body fat percentage on the ketogenic diet
Observations from this graph:
- Body fat percentage came down over the course of the month from 24.2% to 22.9% and followed a similar trend to the loss in weight.
[maxbutton id=”2″]
What’s Going on Here?
This is the outcome I was hoping to see in the early days of the experiment. As my body makes the switch from burning glucose (i.e. carbs) to burning fat (i.e. ketones) for fuel, my blood sugar is coming down and so are my weight and my body fat percentage readings.
As a beginner on Keto, one of the first books I read was called Keto Clarity by Jimmy Moore. This is where I learned about the connection between insulin and weight gain. My take away as a beginner was that the best way to think about losing weight is not to focus on restricting calories, but instead think about trying to restrict your body’s insulin response. The best way to limit insulin release is to limit foods that will spike your blood sugar. Diets like Paleo and Ketogenic are excellent for lowering blood sugar as they replace the foods that spike blood sugar (refined carbs, grains, fruits etc.) with calories from healthy fats that keep blood sugar low yet keep you feeling full and satiated.
Additionally, the weight and body fat loss may be attributed to my body starting to burn fat for fuel instead of glucose, which is one of the many benefits of the ketogenic diet. I also noticed that as my ketone levels increased, my appetite decreased. Ketones are known to act as a a natural appetite suppressant and I found that over the course of the month, I had less food cravings and needed to eat less food in order to feel full.
Still lots to learn but I am very encouraged about my initial experience and intrigued about going deeper into a ketogenic lifestyle.
Up Next
- As of February 1st I’ve also started tracking blood ketones(iv) and will share this data next month
- I will also attempt to obtain a new set of lab tests in February so I can get a sense of what’s happening with my lipid panel and blood sugar markers. I will share this data as soon as I have it.
Thanks for reading. I’d love to hear your thoughts on the above. If you want to track your own health metrics using Heads Up Health, click below to get started.
[maxbutton id=”4″]
Appendix
(i) Blood sugar is being tracked using the Bayer Contour glucometer. I like this meter because the finger lancet is less painful compared to other meters I’ve used.
(ii)(iii) Weight and body fat percentage are being tracked using the Tanita BF679W scale. I like this scale because it’s reasonably priced (50 bucks) and very accurate. I’ve compared the results on this scale to results from an expensive DXA scan and the results typically vary by only 1-2 pounds.
(iv) I am tracking blood ketones using the Precision Xtra blood ketone meter.